Corneal Transplant
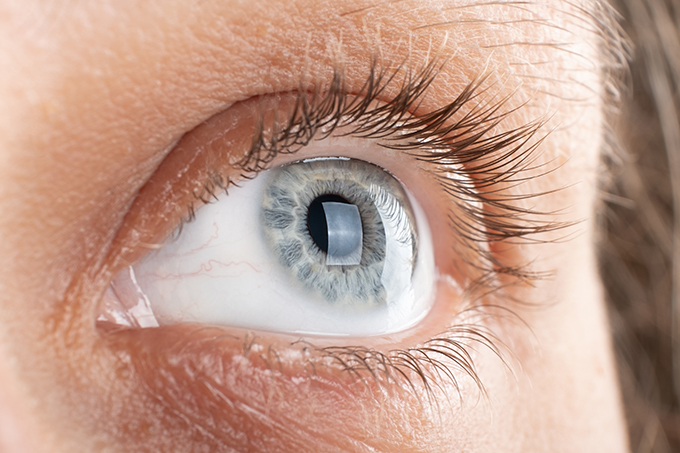
The cornea—the clear, dome-shaped surface at the front of your eye—is essential for sharp, comfortable vision. When this delicate tissue becomes scarred, swollen, or too thin, even the best glasses or contact lenses can’t restore clarity. Modern corneal transplantation offers a highly successful way to replace damaged tissue, restore sight, and dramatically improve quality of life.
Corneal transplantation is unique among medical transplants: almost anyone can be a donor, rejection rates are low, and outcomes continue to improve with advanced surgical techniques.
What is a Corneal Transplant?
A corneal transplantion replaces damaged or diseased corneal tissue with healthy donor tissue. The cornea has several layers, from the outer epithelium to the inner endothelium, and vision depends on each layer remaining clear and smooth.
When scarring, clouding, or distortion affects vision, surgeons may replace the entire cornea or just the specific layer that is not functioning properly.
Take the Next Step
Schedule an appointment to have your cornea evaluated and learn which type of transplant may be right for you.
Who May Need a Corneal Transplant?
A variety of conditions can lead to permanent corneal damage, including:
- Fuchs’ Endothelial Corneal Dystrophy – A common, inherited condition causing gradual degeneration of the inner corneal layer, often starting after age 40.
- Keratoconus – A progressive thinning and bulging of the cornea that can appear in teens and young adults.
- Corneal Infections or Trauma – Injuries, ulcers, or severe infections may leave scarring that blocks vision.
- Swelling After Eye Surgery – Complicated or repeated surgeries sometimes weaken the cornea.
- Glaucoma, uveitis or others eye diseases that can weaken the cornea.
When these issues interfere with daily activities or limit vision, a transplant may be recommended.
What Should Patients Expect?
Corneal transplantation is one of the most successful procedures in ophthalmology, with success rates of around 95% , depending on the health of the eye.
However, surgery is just one part of the journey—patients must commit to:
- Long-term use of prescribed eyedrops
- Regular follow-up visits
- Monitoring for symptoms of rejection
Donor tissue is a true gift, and long-term care helps protect that gift.
Understanding Rejection and Prevention
Unlike other organ transplants, corneal transplants have a very low risk of rejection, and donor-recipient matching is typically not necessary.
Most patients are maintained on a single steroid eyedrop to prevent rejection over time.
Rejection can occur months or even years after surgery. Early treatment is highly effective, so patients should call their provider urgently if they notice:
- Redness
- Light sensitivity
- Pain
- Blurry vision
Prompt evaluation usually allows the graft to recover with medications.
How Technology Has Improved Corneal Transplants
Twenty years ago, corneal transplants often involved replacing the full thickness of the cornea, requiring many stitches and up to a year of healing. Today, Eye Doctors of Washington offers advanced, targeted procedures that replace only the affected layers—leading to:
- Faster recovery
- Fewer complications
- Sharper visual outcomes
For select patients with Fuchs dystrophy, a new technique is available that doesn’t even require donor tissue anymore, decreasing even more the risk of side effects. You can schedule a consultation to know more if you are a good candidate for this technique, abbreviated with DSO or DWEK.
Layer-Specific Transplants
If only the inner layer is damaged—as in Fuchs’ dystrophy—we can perform a Descemet Membrane Endothelial Keratoplasty (DMEK). This surgery replaces only a paper-thin layer of endothelial cells (about 10 microns thick). Vision often returns rapidly, sometimes reaching 20/20 within a month.
If the surface layer is irregular due to partial limbal stem cell insufficiency, we can perform a new kind of transplant, a Descemet membrane anterior keratoplasty (DMAK), which is a non-invasive procedure that helps promote the residual stem cells leading to a clear surface.
Research is currently exploring procedures that will allow us to transplant just the corneal cells themselves.
What is Recovery Like?
Recovery varies based on the type of surgery:
- Full-thickness transplant – Healing can take six months to a year.
- DMEK or partial endothelial transplants – Much faster visual recovery, usually one to three months, but patients must lie flat for a short time after surgery so the new layer seals properly.
Your EDOW surgeon will guide you through each step of your personalized recovery plan and follow-up schedule.
Who Can Donate Corneal Tissue?
Almost anyone can be a corneal donor. Glasses wearers and people who have previously had LASIK can still donate in many cases. Even when tissue isn’t suitable for transplantation, it may be used for research or surgical training—both essential to advancing eye care.
The Impact of Cornea Donation
Corneal donation restores sight—often to two different people, as each donor provides two corneas. Because blindness carries significant social and economic burdens, donating corneal tissue can profoundly improve lives. Many families find comfort in knowing their loved one helped others see again.
Schedule an Appointment
If you’ve been told you have a corneal condition, or you’re struggling with cloudy, distorted vision, our cornea specialists at Eye Doctors of Washington are here to help.
- Schedule an appointment to have your cornea evaluated
- Learn whether a corneal transplant or advanced partial transplant is right for you
- Get a personalized plan to protect and restore your sight
Call our office or request an appointment online today to get started.

